- admin
- 0 Comments
Demystifying the Differences: A Comprehensive Guide to Medical Billing vs. Medical Coding
Are you confused about the differences between medical billing and medical coding? You’re not alone. These two terms are often used interchangeably, causing many people to merge the roles and responsibilities associated with each. However, understanding the distinction between medical billing and medical coding is imperative for anyone working in the healthcare industry or seeking medical services. In this comprehensive guide, we will demystify the differences between medical billing and medical coding, providing you with a clear understanding of their individual functions, methods, and importance within the healthcare system. Whether you’re a healthcare professional looking to boost your knowledge or a patient wanting to better navigate your medical bills, this guide will provide you with the necessary understandings to make informed decisions and warrant precise medical documentation and financial compensation. So, let’s dive in and reveal the mysteries behind this A Comprehensive Guide to Medical Billing vs. Medical Coding.
How to Differentiate between Medical Biller and Medical coder
|
Medical Coder |
Medical biller |
|
Medical coders concentrate on converting medical diagnoses, treatments, and procedures into universally accepted codes. |
Medical billing uses those codes to create insurance claims and bills for patients. |
|
They collaborate with medical staff to confirm accurate coding and documentation. |
They must have deep understanding of medical vocabulary, insurance policies, and billing guidelines. |
|
Medical coders concentrate in transforming medical knowledge into standardized codes |
Medical billers mainly deal with the financial aspects of healthcare |
|
Medical coders require in-depth knowledge of anatomy, physiology, and medical procedures |
Medical billers need expertise in medical terminology, insurance policies, billing regulations, and financial management. |
|
They must be detail-oriented, analytical, and proficient in various coding systems, such as ICD-10-CM and CPT. |
They must possess strong communication and customer service skills to effectively handle patient inquiries and navigate the complex world of insurance claims. |
 Understanding the Roles and Responsibilities of Medical Billers and Medical Coders
Understanding the Roles and Responsibilities of Medical Billers and Medical Coders
Medical billing and medical coding are two separate but interrelated processes that play an essential role in the healthcare industry. To fully understand the differences between the two, it’s important to comprehend the particular responsibilities of medical billers and medical coders.
Medical billers are responsible for interpreting medical services into standardized codes, formulating and presenting claims to insurance companies, and guaranteeing timely reimbursement for healthcare providers. They hold a deep understanding of medical vocabulary, insurance policies, and billing guidelines. Moreover, medical billers are expert in managing patient billing queries, settling claim discrepancies, and keeping accurate financial records.
Additionally, medical coders concentrate on converting medical diagnoses, treatments, and procedures into universally accepted codes. These codes are used for numerous reasons, such as insurance claims, medical study, and statistical analysis. Medical coders must have a solid knowledge of anatomy, physiology, and medical terminology to precisely allocate the suitable codes. They work diligently with healthcare providers, studying medical records and collaborating with medical staff to confirm accurate coding and documentation.
In short, medical billers mainly deal with the financial aspects of healthcare, while medical coders concentrate in transforming medical knowledge into standardized codes. Both roles are crucial for efficient healthcare management and warranting precise reimbursement for healthcare services.
Key Differences between Medical Billing and Medical Coding
Although medical billing and medical coding are closely associated, there are main differences that set them apart. Understanding these differences is necessary for understanding the whole healthcare reimbursement process.
One important distinction lies in the application of each process. Medical billing largely revolves around managing financial aspects, such as insurance claims, billing inquiries, and reimbursement. On the other hand, medical coding is focused around interpreting medical information into standardized codes for numerous purposes, including billing, research, and analysis.
Another significant difference is the skill set required for each role. Medical billers need expertise in medical terminology, insurance policies, billing regulations, and financial management. They must possess strong communication and customer service skills to effectively handle patient inquiries and navigate the complex world of insurance claims. Conversely, medical coders require in-depth knowledge of anatomy, physiology, and medical procedures. They must be detail-oriented, analytical, and proficient in various coding systems, such as ICD-10-CM and CPT.
Furthermore, the timing of medical billing and medical coding also differs. Medical coding typically takes place before medical billing, as the coded information forms the basis for accurate billing and reimbursement. Medical billers use the coded data to prepare claims, submit them to insurance companies, and follow up on payment status. This sequential process ensures that healthcare providers are appropriately compensated for the services rendered.
In summary,
while medical billing and medical coding are interconnected, they have distinct focuses, require different skill sets, and occur at different stages of the healthcare reimbursement process.
 Importance of Accurate Medical Billing and Coding
Importance of Accurate Medical Billing and Coding
Exact medical billing and coding is of utmost importance in the medical industry. Besides the fact that they guarantee legitimate monetary reimbursement for healthcare providers, yet they likewise assume a vital part in patient care, research, and healthcare planning.
From a financial outlook, precise medical billing and coding add to the monetary dependability of healthcare organizations. Appropriate coding guarantees that healthcare providers are reimbursed for the services they deliver, decreasing the chance of income loss. Also, exact billing aids in preventing deceitful activities and guarantees compliance with healthcare regulations and insurance policies.
Besides, precise clinical coding is fundamental for patient care. Appropriate coding permits medical services suppliers to get to extensive and precise patient clinical records, empowering them to go with informed choices in regards to diagnosis, treatment, and medication. Accurate coding also enables effective communication between healthcare professionals, guaranteeing consistent coordination of care.
In the domain of medical research and analysis, correct coding allows for the collection and analysis of healthcare data. This information is crucial for recognizing patterns, assessing treatment results, and further developing medical care quality. Exact coding additionally empowers medical care associations to partake in research studies and add to clinical progressions.
In summary,
accurate medical billing and coding are vital for financial reimbursement, patient care, and healthcare research. They structure the groundwork of a productive medical care framework that benefits both healthcare providers and patients.
 The Process of Medical Billing and Coding
The Process of Medical Billing and Coding
The process of medical billing and coding involves a sequence of steps that commence with patient encounters and end with financial reimbursement. Understanding this interaction is fundamental for knowing the intricacies of medical billing and coding.
The most important phase in the process is the patient encounter. This can be a visit to a healthcare provider’s office, hospital stay, or any other medical service. During the experience, healthcare professionals document the patient’s medical history, symptoms, diagnoses, treatments, and procedures performed. This documentation aids as the basis for medical coding.
Then, medical coders analyse the medical records and interpret the documented report into standardized codes. They use coding systems such as ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification) for diagnoses and CPT (Current Procedural Terminology) for treatments and procedures. Precision and devotion to detail are crucial during this stage to warrant the correct allocation of codes.
When the coding is finished, medical billers utilize the coded data to make claims for submission to insurance companies. This includes gathering the patient’s demographic information, the healthcare provider’s information, and the coded diagnoses, treatments, and procedures. The claim is then submitted electronically or by means of mail to the proper insurance agency.
After submission, medical billers follow up on the claim’s status, confirming that it is administered and reimbursed promptly. They handle any billing requests or inconsistencies that might emerge, working carefully with insurance companies and patients to resolve any issues. Timely and efficient follow-up is pivotal to avoid claim denials or delays in reimbursement.
Finally, once the claim is accepted, the insurance company reimburses the healthcare provider based on the settled upon rates and coverage. Any remaining patient balances are then billed to the patient, and the financial cycle for that particular encounter is complete.
In summary,
the process of medical billing and coding involves patient encounters, medical documentation, coding, claim preparation, submission, follow-up, and reimbursement. It is a complicated and interconnected process that necessitates accuracy and attention to detail.
 Training and Education Requirements for Medical Billers and Medical Coders
Training and Education Requirements for Medical Billers and Medical Coders
To succeed in the fields of medical billing and coding, people must undertake specific training and education to attain the essential knowledge and skills.
For medical billers, formal training isn’t generally obligatory, although it can significantly enhance job prospects and progression prospects. Many ambitious medical billers choose to pursue associate’s or bachelor’s degrees in healthcare administration, medical billing, or a related field. These programs provide a complete understanding of medical terminology, insurance policies, billing regulations, and financial management. Additionally, some universities and vocational schools offer specialized medical billing certificate programs that focus specifically on the complexities of medical billing.
In contrast, medical coders normally require formal training and education to enter the field. Different choices are accessible for ambitious medical coders, including certificate programs, associate’s degrees, and bachelor’s degrees in health information management or medical coding. These programs cover topics such as anatomy, physiology, medical terminology, coding systems, and healthcare regulations. Additionally, aspiring medical coders can pursue industry certifications, such as the Certified Professional Coder (CPC) credential, which displays competence in medical coding.
Continuous education and remaining updated with the up-to-date coding and billing guidelines are critical for both medical billers and medical coders. The healthcare industry is constantly developing, with new coding systems, regulations, and technologies being introduced. By joining workshops, seminars, and online courses, professionals can stay up-to-date of industry changes and enhance their abilities.
In summary,
while formal education is not always mandatory for medical billers, it significantly enhances job possibilities. Medical coders, on the other hand, typically require formal training and education to enter the field. Continuous education and self-improvement are vital for both professions, given the consistently changing nature of the healthcare industry.
Common Challenges and Issues in Medical Billing and Coding
The field of medical billing and coding is not without its challenges and issues. Understanding these difficulties is significant for health care experts and associations to address them effectively and guarantee smooth operations.
One of the most common challenges in medical billing and coding is claim denials. Insurance companies might deny claims in light of multiple factors, like missing information, coding errors, or lack of clinical need. These denials frequently bring about deferred repayment and extra regulatory work for healthcare providers. To alleviate this challenge, medical billers and coders should remain refreshed with the most recent coding rules, accurately document patient information, and maintain open lines of correspondence with insurance agency.
Another challenge is the consistently changing scene of healthcare regulations and coding frameworks. As new coding frameworks, such as ICD-11, are presented, medical coders should adjust and learn new coding conventions. Remaining refreshed with the most recent coding rules and going to attend regular training sessions are essential for accurate coding and compliance.
Additionally, the complexity of insurance policies and billing regulations can pose challenges for medical billers. Each insurance company has its own set of guidelines and obligations, making the billing process complex and time-consuming. Medical billers must be knowledgeable in insurance terminology, coverage limitations, and claim submission procedures to navigate this complexity effectively.
In addition, the change from paper-based clinical records to electronic wellbeing records (EHRs) has presented its own arrangement of difficulties. While EHRs offer various benefits, for example, improved access to patient information and streamlined workflows, healthcare organizations must ensure proper training and execution to avoid data entry errors and system inefficiencies.
In summary,
claim denials, advancing guidelines and coding frameworks, complex insurance contracts, and the progress to EHRs are normal difficulties in medical billing and coding. Addressing these challenges requires continuous education, efficient communication, and a focus on precision and compliance.
Industry Trends and Advancements in Medical Billing and Coding
The field of medical billing and coding is constantly developing, driven by innovative progressions, administrative changes, and the requirement for increased efficiency. Remaining informed about industry patterns is fundamental for experts in this field to adjust and flourish in the ever-changing healthcare landscape.
One significant trend is the increasing adoption of artificial intelligence (AI) and machine learning in medical coding. AI-powered coding software can examine medical records, distinguish potential coding errors, and recommend precise codes in light of past patterns and coding rules. This technology streamlines the coding process, lessens mistakes, and improves coding accuracy.
Another trend is the shift towards value-based care and alternative payment models. Traditional fee-for-service reimbursement is gradually being replaced by payment models that boost quality results and cost reserve funds. Medical billers and coders must adapt to these changes and ensure accurate coding and billing to support value-based care initiatives.
The integration of telehealth and remote patient monitoring into healthcare services has also impacted medical billing and coding. With the expanded utilization of virtual visits and remote checking gadgets, clinical billers and coders should explore the special charging and coding necessities related with these administrations. This includes understanding telehealth reimbursement policies, coding for virtual encounters, and documenting remote monitoring data accurately.
Besides, the push for interoperability and data exchange between healthcare systems has gained momentum. The capacity to consistently share patient data across various medical services suppliers and frameworks is critical for precise coding and billing. Medical billers and coders should stay updated with interoperability standards and leverage technology to ensure efficient data exchange.
In summary,
industry trends such as AI-powered coding software, value-based care, telehealth, and interoperability are molding the fate of medical billing and coding. Adapting to these trends and embracing technological advancements will be vital to outcome in this field.
 Career Opportunities and Growth in the Medical Billing and Coding Field
Career Opportunities and Growth in the Medical Billing and Coding Field
There are several employment prospects in this industry as a result of the growing demand for knowledgeable medical billers and coders. Medical billing and coding specialists are necessary for effective healthcare administration and revenue cycle management as the healthcare sector expands and changes.
Medical billers and coders can work in a variety of healthcare settings, such as clinics, hospitals, doctor’s offices, insurance organisations, and billing and coding firms. Additionally, they have the option of working from home while contracting out their coding and billing services.
The medical billing and coding industry is expected to increase, and there are prospects for specialisation and promotion. Professionals with experience can advance to management or supervisory roles where they are in charge of teams or departments that handle coding and billing. Individuals might also specialise in particular fields.
Additionally, the area of medical billing and coding provides a path for professional development in the management of health information and healthcare administration. An advanced degree or certification in medical billing and coding can offer doors to higher-level roles with more responsibility and leadership chances for professionals with a solid background in these disciplines.
In conclusion,
the medical billing and coding industry offers a wide range of employment options and room for advancement. Professionals with the necessary skills can work in a variety of healthcare settings and can choose to specialise or develop in their current position. For job success in this dynamic field, ongoing education and keeping up with industry changes are essential.
Outsourcing medical billing and coding to specialist like Ibex medical billing will help you so much, to achieve your revenue generation goals. Doctors are the professionals getting the most benefits from the billing organizations.
You can visit our https://ibexmedicalbilling.com/medical-billing-services/
services page for more information. Feel free to contact us.

 Understanding the Roles and Responsibilities of Medical Billers and Medical Coders
Understanding the Roles and Responsibilities of Medical Billers and Medical Coders Importance of Accurate Medical Billing and Coding
Importance of Accurate Medical Billing and Coding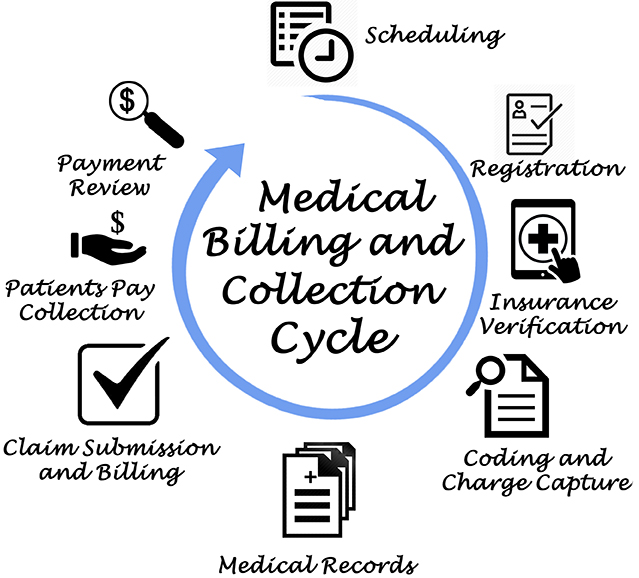 The Process of Medical Billing and Coding
The Process of Medical Billing and Coding Training and Education Requirements for Medical Billers and Medical Coders
Training and Education Requirements for Medical Billers and Medical Coders Career Opportunities and Growth in the Medical Billing and Coding Field
Career Opportunities and Growth in the Medical Billing and Coding Field