PATIENT ELIGIBILITY VERIFICATION
The patient’s eligibility verification for medical billing determines if the patient is eligible to obtain any of the insurance services, coverage and expenses. It is done before any type of service schedule. Eligibility Verification is the first and most significant step of RCM or revenue cycle management. It minimizes claim denials and revenue loss. It improves the patient’s experience as well. You can improve and increase your co-pays and co-insurances. It improves your cash flow and smooths the workflow as well. It boosts your self-pay income.
The disadvantages of not verifying the eligibility criteria of the patients are as follow:
- Inactive and not good insurance policies
- Insecure authorizations result in claim denial and rejections.
- Not defined patient’s financial expenses, which causes surprise bills and panic
- Patients may lose trust and go for another provider.
It is important to improve patient retention for your medical practice as well.
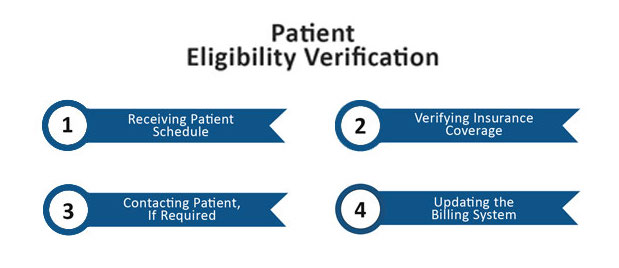
Patients Eligibility verification process:
The process can be a lot easier and quicker if you have a billing platform with immediate eligibility verification. The manual checks by calling and verifying everyone can take a long time which is exhausting. With the help of RTE or Real-Time Eligibility checks, you can save your hours and focus on more important and further steps for insurance services.
The steps are as follows:
- We gather patient’s demographics including their name, date of birth, insurance provider, financial condition, medical records and address etc.
- Our team records and copy insurance card copies.
- The insurance information of patients is added to a suitable tool such as EHR Electronic Health Record, PM Practice Management or RTE etc.
- The different and appropriate services and benefits are selected with the patient’s information electronically to check the eligibility of the patient.
- The following information is identified from the electronic eligibility check:
- The policy holder
- Effective date of the policy
- Term date of the policy if any
- Patient’s co-pay or co-insurance if any
- The deductibles or accumulations of the patient if any
- Patient’s out-of-pocket expenses
- Service pre-authorization requirements if any
- Out of network coverage and payer if any
- Payers contact for authorization if applicable
- Informing the patient about their own expenses
- Patient’s responsibility collection before appointment or treatment
It benefits both the patient and the insurance company.
Advantages for service providers:
- Estimate of patient’s expenses
- Time-saving
- Gathers required verification ahead of time
- Higher claim rates and less errors
Advantages for patients:
- Minimizes stress and estimates an upcoming bill early
- Helps to choose the best among all providers
- Helps to choose the best services
Ibex Medical Billing is a highly professional medical billing and RCM services company. We work globally according to your needs. Our pocket-friendly services give you the best experience of your life. We ensure the best workflow, highly secured communication and scheduling systems. We excel at problem-solving strategies.
Save your precious time and avoid hectic and inflated claim denials by setting up an appointment with us today. We do every work with 100% HIPAA compliance.
Trust us, you won’t be disappointed.